Microbes in Oncology: Controllable Strategies for Bacteria Therapy
1Department of Ultrasound Medicine, Laboratory of Ultrasound Molecular Imaging, The Third Affiliated Hospital of Guangzhou Medical University, Guangzhou, 510000, P. R. China
2CAS Key Laboratory of Quantitative Engineering Biology, Shenzhen Institute of Synthetic Biology, Shenzhen Institutes of Advanced Technology, Chinese Academy of Sciences, Shenzhen, 518055, P. R. China
*Correspondence to: Zhiyi Chen and Fei Yan E-mail: zhiyi_chen@gzhmu.edu.cn; fei.yan@siat.ac.cn
Received: July 2 2020, Revised: August 3 2020, Accepted: September 8 2020, Published Online: November 24 2020
Cite this paper:
Meng Du, Jinsui Yu, Yaozhang Yang, Fei Yan and Zhiyi Chen. Microbes in Oncology: Controllable Strategies for Bacteria Therapy. BIO Integration 2020; 1(4): 185–192.
DOI: 10.15212/bioi-2020-0025. Available at: https://bio-integration.org/
Download citation
© 2020 The Authors. This is an open access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/). See https://bio-integration.org/copyright-and-permissions/
Abstract
Bacterial therapy is an emerging method of tumor treatment. By utilizing wild-type bacteria or engineered bacteria to treat solid tumors, bacterial therapy has recently attracted attention due to its high therapeutic specificity. Although many bacterial strains have been tested in animal models or have even advanced to clinical trials, the efficacy of bacterial therapy remains undesirable. The lack of efficient control methods could cause side effects as well as insufficient therapeutic efficiency, both of which are urgent problems for bacterial therapy. Therefore, some studies have constructed bacteria with inducible plasmid or adsorption with responsive nanoparticles, which improved controllability and specificity during bacterial therapy. Herein, we introduce the unique advantages of bacteria in cancer treatment and highlight the issues associated with the application of bacterial therapy, focusing on the incorporation of various methodologies in the advancement of some controllable strategies in bacterial therapy.
Keywords
Bacteria, controllable approaches, inducible promoter, tumor targeting.
Introduction
Although substantial research has been undertaken to develop new therapies against tumors, the ever-increasing number of cancer cases demonstrates an urgent need for novel therapeutic options. The most common modes for the treatment of cancer include surgery, radiotherapy, and chemotherapy. Although the therapeutic efficiency of surgery is obvious, surgery is invasive and is associated with postoperative complications. Although radiotherapy is suitable for the treatment of solid tumors, it is prone to causing treatment tolerance and surrounding tissue damage. Chemotherapy is widely used in tumor treatment, but the off-target effect of chemotherapy drugs can cause serious toxic side effects to normal tissue. In recent years, biological therapy (i.e., gene therapy, immunotherapy, bacterial therapy, etc.) has attracted widespread attention due to its advantage of low toxicity and lasting curative effects (Table 1) [1].
Table 1 Comparison of Characteristics of Different Therapeutic Modes
| Therapeutic Modality | Types of Tumors | Advantages | Disadvantages |
|---|---|---|---|
| Surgery | Solid tumor | High therapeutic efficiency | Invasive operation, Postoperative complications |
| Radiotherapy | Solid tumor | Local therapy | Therapeutic tolerance, surrounding tissue damage |
| Chemotherapy | All types of tumors | Wide indications | Off-target effect, systemic toxic side effects |
| Biological Therapy | All types of tumors | Curative effect lasting | High cost, dubious curative effect |
The poorly vascularized microenvironments and high interstitial fluid pressures of solid tumors impede the penetration of traditional therapeutic agents into the centers of the cancerous tissue, dramatically reducing their anti-tumor effects [2]. However, these same characteristics of tumor microenvironments provide appropriate conditions for some bacteria to colonize, proliferate, or even develop anti-tumor abilities [3]. In this regard, some bacterial strains have been shown to be advantageous as ideal tumor-targeted delivery systems to transport therapeutic payloads into tumors [4].
Therefore, an apt exploitation of bacteria may provide a valuable solution for overcoming the limitations of other conventional therapies. The past decade has seen the rapid development of bacteria in many cancer treatments [5]. Some engineered bacterial strains have been tested in various preclinical setups and clinical trials. Other reviews have already reported the current stage of bacterial therapy [6, 7]. However, certain urgent issues still need to be considered during clinical translation, especially safety concerns and therapeutic efficiency. To avoid injury to normal tissue caused by constant cytotoxin release of engineered bacteria, some novel strategies such as engineered bacteria with inducible plasmids or responsive nanoparticles have been presented, which could be summarized as controllable bacterial therapy. In this mini-review, the history of bacterial therapy and the challenges faced will be introduced. Furthermore, the research progress of controllable strategies in bacterial therapy will be reviewed.
Mechanism and advantages of bacterial therapy
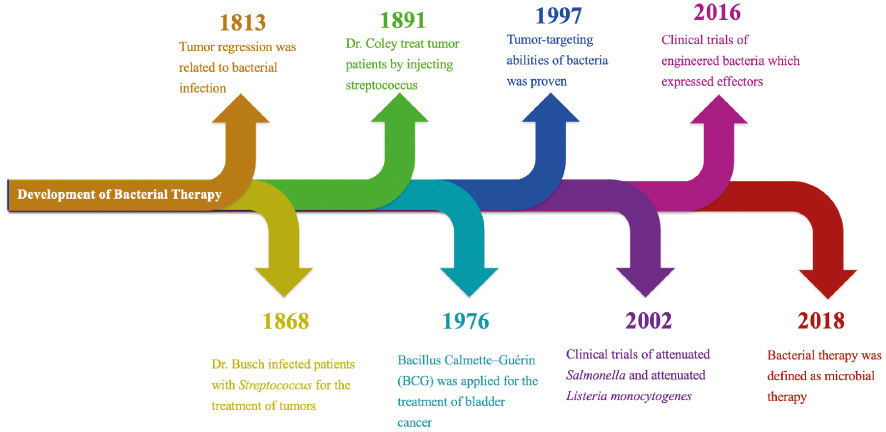
Bacteria have shown great potential in anti-tumor activities since the first documented utilization of therapeutic bacteria to attack cancerous tissue in 1813 (Figure 1). In this case, tumor regression was observed in tumor patients suffering from gas gangrene, which was caused by Clostridia sp. [8]. Later, more clinical reports showed that patients with tumors were cured after the administration of live bacteria. In 1868, Wilhelm Busch infected a patient with malignant sarcoma with Streptococcus pyogenes, and discovered a significant reduction in the volume of tumor [9]. Subsequently, some scholars reported similar cases. William Coley made significant contributions by applying attenuated bacteria for tumor treatment. He was the first to treat malignant sarcoma by injecting Streptococcus into the tumor [10]. At that time, the immune response and high fever caused by bacterial infection were considered to be the main mechanisms for bacterial treatment to achieve anti-tumor effects. With the development of synthetic biology and microbiology, more and more engineered bacterial strains have been developed to improve both the safety and therapeutic efficiency of bacterial therapy. These bacterial strains have also shown great potential in clinical trials. Fortunately, the mechanism of bacterial therapy has been gradually clarified.
Figure 1 Timeline of the development of bacterial therapy.
One of the advantages of bacterial therapy is the good specificity due to the tumor targeting of bacteria. Some bacterial strains such as obligate anaerobes have moderately high tumor specificity. Such bacterial strains tend to accumulate and localize in the tumor region which presents a preferable growth environment (low pH, immune-privileged site) for their proliferation [11]. Tumor-targeting bacteria are therefore ideal vehicles to shuttle therapeutic payloads to tumor tissues [12]. Beyond applying their tumor specificity, certain chemical explorations have also been made to conjugate drug-loaded nanomaterials to tumor-targeting bacteria [13].
Another advantage of bacterial therapy is the ability of immunomodulatory activities caused by bacteria [14]. During bacterial therapy, tumor regression occurs in response to multiple therapeutic effects, including adjuvant effects of tumor immune surveillance and direct cytotoxicity of engineered bacteria. As exogenous species, bacteria can intrinsically cause innate immune responses [15]. Inspired by the immunomodulatory activities, some bacterial strains have been engineered to express specific tumor antigens on their surfaces and applied as “cancer vaccines,” activating tumor-specific immune responses [16]. For instance, the CRS-207 vaccine, which was engineered to express mesothelin by deleting the genes of actA and inlB, demonstrated the capacity to activate the immune response of NK cells and T cells to kill cancer cells [17].
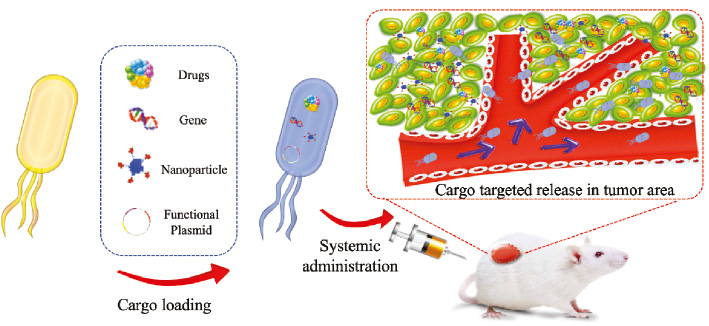
Since bacteria have the capabilities of tumor targeting and immune activation, the treatment mode of bacterial therapy is diverse. According to existing research, bacteria can be used as special biological carriers to deliver drugs [18], genes [19], and nanoparticles [20, 21] to tumor regions, enhancing the anti-tumor efficiency (Figure 2). Furthermore, some genetically engineered bacteria can even express and release therapeutic molecules in tumor microenvironments to achieve ideal anti-tumor effects [22]. For instance, Schlechte et al. developed engineered Clostridium with recombinant plasmid encoding colicin E3, and proved that the recombined bacteria could express E3 to inhibit protein synthesis of tumor cells [23]. Additionally, Thamm et al. reported that the genetically modified bacteria of Salmonella typhimurium VNP20009, which were attenuated by chromosomal deletion of the purI and msbB genes, resulted in tumor regression in cancerous dog models after weekly or biweekly intravenous administration [24].
Figure 2 Bacteria as a vector for the delivery of a therapeutic substance. With the characteristics of tumor targeting, bacteria could be applied as a vector for the delivery of drugs, functional nanoparticles, and therapeutics. Also, bacteria which were transformed with functional plasmids carrying gene expression cassettes could express therapeutic proteins.
Safety concern of bacterial therapy
With the development of biomedical research as well as bacterial behavior and genetic engineering, some attenuated bacteria have been widely applied in clinical applications, such as Bacillus–Calmette–Guérin (BCG). BCG is a classical bacterial vaccine, which is composed of attenuated bovine tuberculosis bacillus [25]. Due to its immunomodulatory capabilities, BCG has been applied in the treatment of bladder cancer. However, it was reported that BCG could cause hematuria and fever during treatment [26].
Safety is a major limitation of bacterial therapy. Further clinical application of utilizing bacteria in cancer treatment has mainly been impeded due to safety concerns. A discontinued phase I trial in 2016 using ADXS11-001 (Axalimogene filolisbac) in human papillomavirus (HPV)-positive oropharyngeal cancer (OPC) once again heightened the importance of safety concerns and received considerable critical attention [27]. The side effects of bacterial therapy are mainly caused by protein toxins and the payload released by bacteria. To reduce the toxicity of bacteria, some attenuated strains, such as VNP20009 [28], CRS-207 [29], and so on, were developed. To avoid the toxicity of the payload released by engineered bacteria, the process of bacterial therapy, especially the gene expression in engineered bacteria, should be carefully managed.
Controllable bacterial therapy
The most straightforward method to increase anti-tumor activity would be to engineer bacteria-expressing cytotoxic agents [30, 31]. However, a major problem for the application of cytotoxin-expressing bacteria in cancer treatment is their intrinsic toxicity in non-tumoral reticuloendothelial organs, mainly the liver and spleen, due to their initial localization in these organs after systematic administration [32]. The constitutive payload expression would thus inevitably result in hepatic or splenic injury, reducing the therapeutic efficiency of the engineered bacteria. In addition, unlike nanoparticles or other common vectors for drug delivery, bacteria, as live vectors, need to retain their activity and ability to express payloads for the desirable delivery of therapeutic payloads. Some scholars pointed out that constitutive payload expression could cause metabolic burdens, thus decreasing the fitness and therapeutic efficiency of engineered bacteria [33]. With the development of bacterial genetics, the strategy of engineering bacteria with inducible expression system was proposed and it provided a novel idea for controllable bacterial therapy (Table 2).
Table 2 Representative Modes of Controllable Bacterial Therapy
| Type | Effector System | Inducible Factor | Characteristics | Refs |
|---|---|---|---|---|
| Chemical controllable | pBAD plasmid | L-arabinose | High efficiency | [31, 35–38] |
| pET28a plasmid | IPTG | High efficiency | 20 | |
| Environment controllable | STM1781 promoter | pH | Safety | 40 |
| PpepT promoter | Hypoxia | Safety | 43 | |
| Physical controllable | recA promoter | Radiation | High specificity | 44 |
| pBV220 plasmid and gold nanoparticles | Light irradiation | High specificity | 46 | |
| Quorum-sensing controllable | Quorum-sensing gene circuit | AHL | Internal trigger | [47–49] |
Chemical controllable strategy
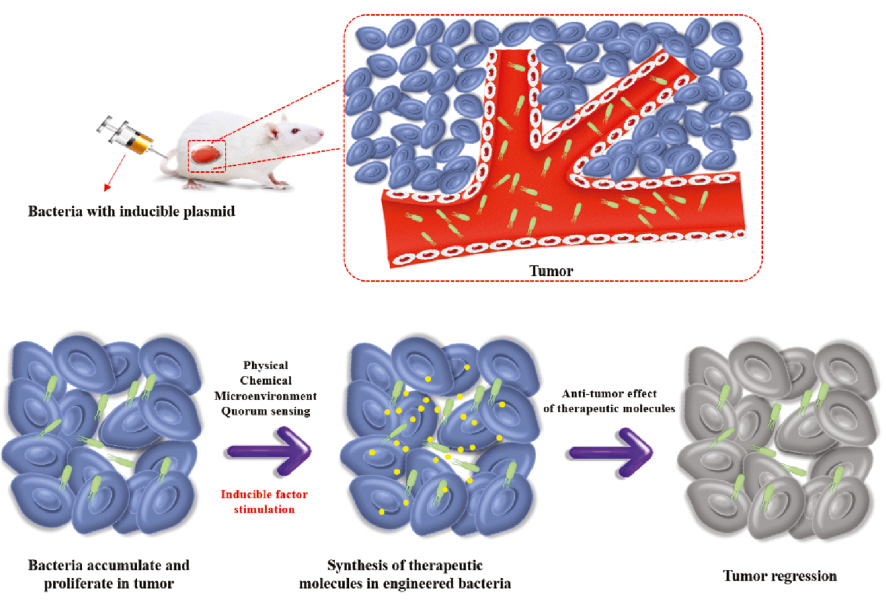
Some efforts have been made to solve the problems by using inducible promoter systems in genetic engineering for better control of bacterial gene expression to decrease toxicity to normal tissues (Figure 2). Chemical-inducible promoter systems are most often used in protein engineering research. The expression of the proteins of interest can be controlled by the administration of a chemical compound such as isopropyl β-D-thiogalactoside (IPTG), arabinose, and so on [34]. Based on this principle, some bacterial strains were engineered with a chemical-inducible promoter system to enhance the controllability of the expression of therapeutic molecules in bacterial therapy (Figure 3).
Figure 3 Schematic of controllable bacterial therapy. After the bacteria with the inducible plasmid is administrated systemically, bacteria could accumulate and proliferate in the tumor due to its tumor targeting ability. Then with the stimulation of a physical trigger, a chemical trigger, the conditions of the tumor microenvironment and the quorum sensing, engineered bacteria could synthesis and release the therapeutic molecules in situ to realize tumor targeting treatment.
PBAD is a classic inducible plasmid that activates the expression of target genes in response to L-arabinose. In 2007, Stritzker et al. inserted PBAD plasmids encoding luciferase into Escherichia coli strain Nissle 1917. The results demonstrated that induced-light emission from the bacterial luciferase within tumor-bearing mice could only be detected after arabinose injection, which provided the fundamental basis for chemical controllable strategy for bacterial therapy [35]. Hereafter, Jung-Joon Min and colleagues performed other research involving the application of PBAD engineered bacteria in tumor treatment [36]. By utilizing the induction system of the L-arabinose-dependent promoter PBAD for gene activation, the engineered bacteria could express and release therapeutic molecules in the tumor area under the control of arabinose administration and achieve ideal therapeutic efficiency [31, 36–38].
Tumor microenvironment-triggered bacterial therapy
There are significant differences between the tumor microenvironment and the internal environment of the human body in terms of physical and chemical properties, such as hypoxia and low pH [39]. Acidic pH in a tumor microenvironment plays an important role in tumor progression via immune suppression and drug resistance. In another way, it could also be applied as a trigger for controllable bacterial therapy. After screening the S. typhimurium library, Fliente et al. found that the STM1787 promoter was sensitive to the acidic microenvironment of tumors. Furthermore, they constructed Salmonella which expressed Shiga toxin under the control of the STM1787 promoter. The recombined strains showed dramatic anti-tumor effects in vitro and in vivo, due to the characteristics of acidic feature in tumor microenvironment [40].
Hypoxia is an acknowledged feature of solid tumors. In this regard, bacteria engineered with a hypoxia-inducible system also has great potential in the treatment of tumors [41, 42]. In one case, by placing a critical gene under a hypoxia-conditioned promoter, S. typhimurium strain SL7207 was engineered to survive only in anaerobic conditions (strain YB1) without otherwise affecting its functions. The results revealed that YB1 served as a safe bacterial vector for anti-tumor therapies without compromising other functions or tumor fitness of the bacteria as attenuation methods normally do [43].
Physical controllable strategy
In addition to the strategy mentioned, the physical controllable strategy also shows great potential in controllable bacterial therapy due to its characteristics of good specificity. With the stimulation of physical triggers, anti-tumor agents could be synthesized in tumor areas, which could reduce the toxicity in normal tissues. Therefore, some studies utilized physical stimulation to achieve spatiotemporal control of the gene expression of bacteria for targeted tumor therapy. Nuyts et al. used radiation-induced recA promoter to control the expression of lacZ (a therapeutic gene). As a result, under the control of recA promoter, β-galactosidase activity was significantly increased to improve therapeutic effect after 2 Gy of irradiation [44].
In addition to the method of genetic modification, decoration of responsive nanoparticles also provided a new physical-controllable strategy for bacterial therapy [45]. Fan et al. constructed a thermally biotic/abiotic hybrid system, which was composed of gold nanoparticles and engineered E. coli carrying thermally sensitive plasmid pBV220 expressing tumor necrosis factor-alpha (TNF-α). Based on the tumor targeting of E. coli, gold nanoparticles-loaded bacteria could accumulate in tumor tissue after administration orally. Under light irradiation, the photothermal effect produced by gold nanoparticles could activate the expression of TNF-α from engineered E. coli, which resulted in ideal local anti-tumor effects. The research implied that the integration of nanomedicine and synthetic biology provide a novel strategy for controllable bacterial therapy [46].
Quorum sensing regulating strategy
Some bacterial strains such as Salmonella were proven to express proteins only in tightly packed colonies within tumors, showing a density-dependent characteristic [47]. In 2016, Tal Danino et al. proposed an interesting idea of using the proliferation characteristics of bacteria itself as a trigger for payload release. Exploiting the natural propensity for certain bacteria to colonize tumor sites, they designed a quorum-sensing gene circuit for a transcriptional program enabling effective bacterial population control and drug release in repeated cycles. When the concentration of acyl-homoserine lactone (AHL) released by bacteria reached a certain threshold, the bacteria would split and promote drug release. After lysis, a few remaining bacteria reproduced and repeated the cycle(s). The results revealed that the circuit-engineered bacteria had notable anti-tumor activity and caused prolonged survival of tumor-bearing mice [48]. Based on the advantages of this system, in 2019, this group engineered E. coli to specifically lyse in the tumor area and release the encoded nanobody antagonist of CD47. Compared with conventional systemic treatments, the recombinant strain improved the targeted therapeutic effect of the CD47-antibody, induced tumor regression and systemic anti-tumor immunity. The biological control switch strategy to synchronously lyse at a threshold population density may provide a promising solution to precisely control drug delivery or other therapeutic effects [49].
Prospects of bacterial therapy
With the rapid advancement of cancer research since the 19th century, bacterial therapy has progressed to clinical trials. In 2002, a clinical trial involving bacterial therapy was raised by the National Cancer Institute in USA. In this trial, 24 patients received administration of VNP20009, which is a strain of attenuated Salmonella. It was proven that VNP20009 was safe and it could colonize in tumor areas at a high dose of administration [50]. Later, some strains of bacteria engineered with effectors were also applied in clinical trials [51, 52]. Overall, the results of these clinical trials revealed that engineered bacteria were proven to be safely administrated [53, 54]. However, according to these clinical trials, the effects of bacterial therapy alone was not promising.
The pathogenesis of tumors is complex. Monotherapy often fails to achieve the desired therapeutic effect. Therefore, the combination of multiple therapeutic modes is widely applied in clinical practice. Combination therapy can overcome the shortcomings of monotherapy, reduce the therapeutic dose, and improve the sensitivity of tumor treatment. It has been proven that the combination of engineered bacteria and chemotherapy as well as radiotherapy could significantly inhibit the growth of tumors, which is mainly due to the immunity response caused by engineered bacteria in tumor areas, enhancing the sensitivity of traditional cancer treatment and reducing the risk of tumor recurrence [55, 56]. In 2019, a new clinical trial report also confirmed this conclusion. In this study, 35 patients with advanced peritoneal mesothelioma received standard chemotherapy and CRS-207, an attenuated Listeria monocytogenes strain expressing mesothelin. As a result, the rate of disease control and therapeutic reactivity reached 89% and 54%, respectively [57]. However, the strategy of bacteria-based combination treatment still requires further optimization in several aspects, including the ratio of engineered bacteria to drugs, the timing of bacterial administration, and so on.
Due to safety concerns, there are still some challenges for bacterial therapy. Since live bacteria could have both therapeutic and toxic effects, it is necessary to maintain the balance of tumor therapeutic outcomes with the risk of possible serious infection caused by bacteria [7]. It may be feasible to monitor the process of bacterial therapy with reporter gene imaging technique. For this purpose, some researchers modified bacteria with various reporter genes, which were monitored by different imaging techniques including optical imaging [58], positron emission tomography [59], and magnetic resonance imaging [60]. In this regard, the imaging signals of bacteria could provide information about their distribution and proliferation, which provides a non-invasive monitoring method for bacterial therapy.
Conclusion
Bacterial therapy shows great potential for application in tumor treatment. However, the relatively low therapeutic efficiency and safety risks halts its further clinical application. One potential solution is to develop controllable strategies for bacterial therapy through engineered bacteria with inducible plasmid and responsive nanoparticles. Controllable approaches in bacterial therapy present a necessity for achieving better therapeutic outcomes. The approaches mentioned exemplify a methodology for applying synthetic biology to exploit the inherent features of certain bacteria to target, selectively colonize, and eventually exert anti-tumor effects. It is believed that with the continuous development of synthetic biology and molecular cloning technology, more new strains of high efficiency and safety will be developed and applied to clinical practice, which will provide new paths to improve the efficiency of tumor treatment.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (No. 81971621, No. 81671707), Natural Science Foundation of Guangdong Province (No. 2018A030313678, No. 2019A1515012212), Research Fund for Lin He’s Academician Workstation of New Medicine and Clinical Translation and Youth Foundation of Scientific Research of The Third Affiliated Hospital of Guangzhou Medical University (No. 2018Q03).
References
- Schirrmacher V. From chemotherapy to biological therapy: a review of novel concepts to reduce the side effects of systemic cancer treatment (Review). Int J Oncol 2019;54:407-19. [PMID: 30570109 DOI: 10.3892/ijo.2018.4661]
- Fokas E, McKenna WG, Muschel RJ. The impact of tumor microenvironment on cancer treatment and its modulation by direct and indirect antivascular strategies. Cancer Metastasis Rev 2012;31:823-42. [PMID: 22825313 DOI: 10.1007/s10555-012-9394-4]
- Forbes NS. Engineering the perfect (bacterial) cancer therapy. Nat Rev Cancer 2010;10:785-94. [PMID: 20944664 DOI: 10.1038/nrc2934]
- Felgner S, Kocijancic D, Frahm M, Weiss S. Bacteria in cancer therapy: renaissance of an old concept. Int J Microbiol 2016;2016:8451728. [PMID: 27051423 DOI: 10.1155/2016/8451728]
- Duong MT, Qin Y, You SH, Min JJ. Bacteria-cancer interactions: bacteria-based cancer therapy. Exp Mol Med 2019;51:1-15. [PMID: 31827064 DOI: 10.1038/s12276-019-0297-0]
- Sedighi M, Zahedi Bialvaei A, Hamblin MR, Ohadi E, Asadi A, et al. Therapeutic bacteria to combat cancer; current advances, challenges, and opportunities. Cancer Med 2019;8:3167-181. [PMID: 30950210 DOI: 10.1002/cam4.2148]
- Zhou S, Gravekamp C, Bermudes D, Liu K. Tumour-targeting bacteria engineered to fight cancer. Nat Rev Cancer 2018;18:727-43. [PMID: 30405213 DOI: 10.1038/s41568-018-0070-z]
- McCarthy EF. The toxins of William B. Coley and the treatment of bone and soft-tissue sarcomas. Iowa Orthop J 2006;26:154-8. [PMID: 16789469]
- Pawelek JM, Low KB, Bermudes D. Bacteria as tumour-targeting vectors. Lancet Oncol 2003;4:548-56. [PMID: 12965276 DOI: 10.1016/s1470-2045(03)01194-x]
- Coley WB. II. Contribution to the knowledge of sarcoma. Ann Surg 1891;14:199-220. [PMID: 17859590 DOI: 10.1097/00000658-189112000-00015]
- Zoaby N, Shainsky-Roitman J, Badarneh S, Abumanhal H, Leshansky A, et al. Autonomous bacterial nanoswimmers target cancer. J Control Release 2017;257:68-75. [PMID: 27744036 DOI: 10.1016/j.jconrel.2016.10.006]
- Gardlik R, Fruehauf JH. Bacterial vectors and delivery systems in cancer therapy. IDrugs 2010;13:701-6. [PMID: 20878592]
- Chen W, Wang Y, Qin M, Zhang X, Zhang Z, et al. Bacteria-driven hypoxia targeting for combined biotherapy and photothermal therapy. ACS Nano 2018;12:5995-6005. [PMID: 29786420 DOI: 10.1021/acsnano.8b02235]
- Felgner S, Kocijancic D, Frahm M, Heise U, Rohde M, et al. Engineered Salmonella enterica serovar Typhimurium overcomes limitations of anti-bacterial immunity in bacteria-mediated tumor therapy. Oncoimmunology 2018;7:e1382791. [PMID: 29308303 DOI: 10.1080/2162402X.2017.1382791]
- Nallar SC, Xu DQ, Kalvakolanu DV. Bacteria and genetically modified bacteria as cancer therapeutics: current advances and challenges. Cytokine 2017;89:160-72. [PMID: 26778055 DOI: 10.1016/j.cyto.2016.01.002]
- Bereta M, Hayhurst A, Gajda M, Chorobik P, Targosz M, et al. Improving tumor targeting and therapeutic potential of Salmonella VNP20009 by displaying cell surface CEA-specific antibodies. Vaccine 2007;25:4183-92. [PMID: 17399861 DOI: 10.1016/j.vaccine.2007.03.008]
- Hassan R, Thomas A, Alewine C, Le DT, Jaffee EM, et al. Mesothelin immunotherapy for cancer: ready for prime time? J Clin Oncol 2016;34:4171-9. [PMID: 27863199 DOI: 10.1200/JCO.2016.68.3672]
- Xie S, Zhao L, Song X, Tang M, Mo C, et al. Doxorubicin-conjugated Escherichia coli Nissle 1917 swimmers to achieve tumor targeting and responsive drug release. J Control Release 2017;268:390-9. [PMID: 29101053 DOI: 10.1016/j.jconrel.2017.10.041]
- Vassaux G, Nitcheu J, Jezzard S, Lemoine NR. Bacterial gene therapy strategies. J Pathol 2006;208:290-8. [PMID: 16362987 DOI: 10.1002/path.1865]
- Fan JX, Peng MY, Wang H, Zheng HR, Liu ZL, et al. Engineered bacterial bioreactor for tumor therapy via Fenton-like reaction with localized H2O2 generation. Adv Mater 2019;31:e1808278. [PMID: 30803049 DOI: 10.1002/adma.201808278]
- Chen Y, Du M, Yu J, Rao L, Chen X, et al. Nanobiohybrids: a synergistic integration of bacteria and nanomaterials in cancer therapy. BIO Integration 2020;1:25–36. [DOI: 10.15212/bioi-2020-0008]
- Song S, Vuai MS, Zhong M. The role of bacteria in cancer therapy – enemies in the past, but allies at present. Infect Agent Cancer 2018;13:9. [PMID: 29568324 DOI: 10.1186/s13027-018-0180-y]
- Schlechte H, Elbe B. Recombinant plasmid DNA variation of Clostridium oncolyticum – model experiments of cancerostatic gene transfer. Zentralbl Bakteriol Mikrobiol Hyg A 1988;268:347-56. [PMID: 3043982 DOI: 10.1016/s0176-6724(88)80019-1]
- Thamm DH, Kurzman ID, King I, Li Z, Sznol M, et al. Systemic administration of an attenuated, tumor-targeting Salmonella typhimurium to dogs with spontaneous neoplasia: phase I evaluation. Clin Cancer Res 2005;11:4827-34. [PMID: 16000580 DOI: 10.1158/1078-0432.CCR-04-2510]
- Herr HW, Schwalb DM, Zhang ZF, Sogani PC, Fair WR, et al. Intravesical bacillus Calmette–Guerin therapy prevents tumor progression and death from superficial bladder cancer: ten-year follow-up of a prospective randomized trial. J Clin Oncol 1995;13:1404-8. [PMID: 7751885 DOI: 10.1200/JCO.1995.13.6.1404]
- Morales A, Eidinger D, Bruce AW. Intracavitary bacillus Calmette–Guerin in the treatment of superficial bladder tumors. J Urol 2017;197:S142-5. [PMID: 28012770 DOI: 10.1016/j.juro.2016.10.101]
- Sacco JJ, Evans M, Harrington KJ, Man S, Powell N, et al. Systemic listeriosis following vaccination with the attenuated Listeria monocytogenes therapeutic vaccine, ADXS11-001. Hum Vaccin Immunother 2016;12:1085-6. [PMID: 26618528 DOI: 10.1080/21645515.2015.1121338]
- Liang K, Liu Q, Li P, Luo H, Wang H, et al. Genetically engineered Salmonella Typhimurium: recent advances in cancer therapy. Cancer Lett 2019;448:168-81. [PMID: 30753837 DOI: 10.1016/j.canlet.2019.01.037]
- Le DT, Brockstedt DG, Nir-Paz R, Hampl J, Mathur S, et al. A live-attenuated Listeria vaccine (ANZ-100) and a live-attenuated Listeria vaccine expressing mesothelin (CRS-207) for advanced cancers: phase I studies of safety and immune induction. Clin Cancer Res 2012;18:858-68. [PMID: 22147941 DOI: 10.1158/1078-0432.CCR-11-2121]
- Yoon W, Park YC, Kim J, Chae YS, Byeon JH, et al. Application of genetically engineered Salmonella typhimurium for interferon-gamma-induced therapy against melanoma. Eur J Cancer 2017;70:48-61. [PMID: 27883926 DOI: 10.1016/j.ejca.2016.10.010]
- Wen M, Zheng JH, Choi JM, Pei J, Li CH, et al. Genetically-engineered Salmonella typhimurium expressing TIMP-2 as a therapeutic intervention in an orthotopic glioma mouse model. Cancer Lett 2018;433:140-6. [PMID: 29959056 DOI: 10.1016/j.canlet.2018.06.031]
- Galen JE, Levine MM. Can a ‘flawless’ live vector vaccine strain be engineered? Trends Microbiol 2001;9:372-6. [PMID: 11514219 DOI: 10.1016/s0966-842x(01)02096-0]
- Wu G, Yan Q, Jones JA, Tang YJ, Fong SS, et al. Metabolic burden: cornerstones in synthetic biology and metabolic engineering applications. Trends Biotechnol 2016;34:652-64. [PMID: 26996613 DOI: 10.1016/j.tibtech.2016.02.010]
- Kim NM, Sinnott RW, Sandoval NR. Transcription factor-based biosensors and inducible systems in non-model bacteria: current progress and future directions. Curr Opin Biotechnol 2019;64:39-46. [PMID: 31669680 DOI: 10.1016/j.copbio.2019.09.009]
- Stritzker J, Weibel S, Hill PJ, Oelschlaeger TA, Goebel W, et al. Tumor-specific colonization, tissue distribution, and gene induction by probiotic Escherichia coli Nissle 1917 in live mice. Int J Med Microbiol 2007;297:151-62. [PMID: 17448724 DOI: 10.1016/j.ijmm.2007.01.008]
- Nguyen VH, Kim HS, Ha JM, Hong Y, Choy HE, et al. Genetically engineered Salmonella typhimurium as an imageable therapeutic probe for cancer. Cancer Res 2010;70:18-23. [PMID: 20028866 DOI: 10.1158/0008-5472.CAN-09-3453]
- Park SH, Zheng JH, Nguyen VH, Jiang SN, Kim DY, et al. RGD Peptide cell-surface display enhances the targeting and therapeutic efficacy of attenuated Salmonella-mediated cancer therapy. Theranostics 2016;6:1672-82. [PMID: 27446500 DOI: 10.7150/thno.16135]
- Zheng JH, Nguyen VH, Jiang SN, Park SH, Tan W, et al. Two-step enhanced cancer immunotherapy with engineered Salmonella typhimurium secreting heterologous flagellin. Sci Transl Med 2017;9. [PMID: 28179508 DOI: 10.1126/scitranslmed.aak9537]
- Wu T, Dai Y. Tumor microenvironment and therapeutic response. Cancer Lett 2017;387:61-8. [PMID: 26845449 DOI: 10.1016/j.canlet.2016.01.043]
- Fliente K, Kocher B, Gammon ST, Novack DV, McKinney JS, et al. A bioluminescent transposon reporter-trap identifies tumor-specific microenvironment-induced promoters in Salmonella for conditional bacterial-based tumor therapy. Cancer Discov 2012;2:624-37. [PMID: 22728436 DOI: 10.1158/2159-8290.CD-11-0201]
- Arrach N, Zhao M, Porwollik S, Hoffman RM, McClelland M. Salmonella promoters preferentially activated inside tumors. Cancer Res 2008;68:4827-32. [PMID: 18559530 DOI: 10.1158/0008-5472.CAN-08-0552]
- Leschner S, Deyneko IV, Lienenklaus S, Wolf K, Bloecker H, et al. Identification of tumor-specific Salmonella Typhimurium promoters and their regulatory logic. Nucleic Acids Res 2012;40:2984-94. [PMID: 22140114 DOI: 10.1093/nar/gkr1041]
- Yu B, Yang M, Shi L, Yao Y, Jiang Q, et al. Explicit hypoxia targeting with tumor suppression by creating an “obligate” anaerobic Salmonella Typhimurium strain. Sci Rep 2012;2:436. [PMID: 22666539 DOI: 10.1038/srep00436]
- Nuyts S, Van Mellaert L, Theys J, Landuyt W, Lambin P, et al. The use of radiation-induced bacterial promoters in anaerobic conditions: a means to control gene expression in Clostridium-mediated therapy for cancer. Radiat Res 2001;155:716-23. [PMID: 11302769 DOI: 10.1667/0033-7587(2001)155[0716:tuorib]2.0.co;2]
- Zheng DW, Chen Y, Li ZH, Xu L, Li CX, et al. Optically-controlled bacterial metabolite for cancer therapy. Nat Commun 2018;9:1680. [PMID: 29700283 DOI: 10.1038/s41467-018-03233-9]
- Fan JX, Li ZH, Liu XH, Zheng DW, Chen Y, et al. Bacteria-mediated tumor therapy utilizing photothermally-controlled TNF-alpha expression via oral administration. Nano Lett 2018;18:2373-80. [PMID: 29558152 DOI: 10.1021/acs.nanolett.7b05323]
- Swofford CA, Van Dessel N, Forbes NS. Quorum-sensing Salmonella selectively trigger protein expression within tumors. Proc Natl Acad Sci U S A 2015;112:3457-62. [PMID: 25737556 DOI: 10.1073/pnas.1414558112]
- Din MO, Danino T, Prindle A, Skalak M, Selimkhanov J, et al. Synchronized cycles of bacterial lysis for in vivo delivery. Nature 2016;536:81-5. [PMID: 27437587 DOI: 10.1038/nature18930]
- Chowdhury S, Castro S, Coker C, Hinchliffe TE, Arpaia N, et al. Programmable bacteria induce durable tumor regression and systemic antitumor immunity. Nat Med 2019;25:1057-63. [PMID: 31270504 DOI: 10.1038/s41591-019-0498-z]
- Toso JF, Gill VJ, Hwu P, Marincola FM, Restifo NP, et al. Phase I study of the intravenous administration of attenuated Salmonella typhimurium to patients with metastatic melanoma. J Clin Oncol 2002;20:142-52. [PMID: 11773163 DOI: 10.1200/JCO.2002.20.1.142]
- Schmitz-Winnenthal FH, Hohmann N, Schmidt T, Podola L, Friedrich T, et al. A phase 1 trial extension to assess immunologic efficacy and safety of prime-boost vaccination with VXM01, an oral T cell vaccine against VEGFR2, in patients with advanced pancreatic cancer. Oncoimmunology 2018;7:e1303584. [PMID: 29632710 DOI: 10.1080/2162402X.2017.1303584]
- Nemunaitis J, Cunningham C, Senzer N, Kuhn J, Cramm J, et al. Pilot trial of genetically modified, attenuated Salmonella expressing the E. coli cytosine deaminase gene in refractory cancer patients. Cancer Gene Ther 2003;10:737-44. [PMID: 14502226 DOI: 10.1038/sj.cgt.7700634]
- Le DT, Wang-Gillam A, Picozzi V, Greten TF, Crocenzi T, et al. Safety and survival with GVAX pancreas prime and Listeria Monocytogenes-expressing mesothelin (CRS-207) boost vaccines for metastatic pancreatic cancer. J Clin Oncol 2015;33:1325-33. [PMID: 25584002 DOI: 10.1200/JCO.2014.57.4244]
- Heimann DM, Rosenberg SA. Continuous intravenous administration of live genetically modified Salmonella typhimurium in patients with metastatic melanoma. J Immunother 2003;26:179-80. [PMID: 12616110 DOI: 10.1097/00002371-200303000-00011]
- Lee CH, Wu CL, Tai YS, Shiau AL. Systemic administration of attenuated Salmonella choleraesuis in combination with cisplatin for cancer therapy. Mol Ther 2005;11:707-6. [PMID: 15851009 DOI: 10.1016/j.ymthe.2005.01.008]
- Jiang SN, Phan TX, Nam TK, Nguyen VH, Kim HS, et al. Inhibition of tumor growth and metastasis by a combination of Escherichia coli-mediated cytolytic therapy and radiotherapy. Mol Ther 2010;18:635-42. [PMID: 20051939 DOI: 10.1038/mt.2009.295]
- Hassan R, Alley E, Kindler H, Antonia S, Jahan T, et al. Clinical response of live-attenuated, Listeria monocytogenes expressing mesothelin (CRS-207) with chemotherapy in patients with malignant pleural mesothelioma. Clin Cancer Res 2019;25:5787-98. [PMID: 31263030 DOI: 10.1158/1078-0432.CCR-19-0070]
- Yu YA, Shabahang S, Timiryasova TM, Zhang Q, Beltz R, et al. Visualization of tumors and metastases in live animals with bacteria and vaccinia virus encoding light-emitting proteins. Nat Biotechnol 2004;22:313-20. [PMID: 14990953 DOI: 10.1038/nbt937]
- Brader P, Stritzker J, Riedl CC, Zanzonico P, Cai S, et al. Escherichia coli Nissle 1917 facilitates tumor detection by positron emission tomography and optical imaging. Clin Cancer Res 2008;14:2295-302. [PMID: 18369089 DOI: 10.1158/1078-0432.CCR-07-4254]
- Hill PJ, Stritzker J, Scadeng M, Geissinger U, Haddad D, et al. Magnetic resonance imaging of tumors colonized with bacterial ferritin-expressing Escherichia coli. PLoS One 2011;6:e25409. [PMID: 21984917 DOI: 10.1371/journal.pone.0025409]